Now that we’ve shed some light on the brain and Alzheimer’s in the Understanding Alzheimer’s Disease article, let’s focus on the genetics and risk factors for developing dementia and Alzheimer’s.
Genetics
In the case of Alzheimer’s, some genes are thought to be the cause in about 1% of cases. About twenty genes would increase the risks. The most important genetic risk factor is the APOE4 gene: 1 copy of the gene = 3 to 4 times more risk, 2 copies of the gene = 10 times more risk.
Of course we have two copies of each of our genes, one copy from our mother, and one copy from our father. In all Alzheimer’s cases, 25% of people would have a copy of APOE4, 2% would have both. There would therefore be approximately 30% of the cases which would be of genetic dependence.
In a recent publication from Harvard University regarding genetic risks and family inheritance, it was mentioned that the presence of a case in the family should not worry us more than that. The risks of developing the disease are 2% per year from the age of 65 and 5% per year from the age of 70. For someone with a close family member who is affected, there is talk of a 30% increase in this risk. This means 2.6% from the age of 65 and 6.5% from the age of 70. The 30% applies to medium risk.
Fortunately, healthy lifestyles can greatly reduce this risk even among those who carry the gene. No matter our genetics, we should pay attention to all the risk factors.
Blood circulation and the brain
Remember that the hippocampus (the seat of memory) may be affected in the first place by Alzheimer’s due to its proximity to the arteries that supply the brain. The effect of the increase in blood pressure would therefore be greater in the small blood vessels that feed the hippocampus.
The reality of the fragile blood circulation in the brain allows us to better understand all the risk factors. Anything that can weaken or risk blocking blood vessels increases the risk of dementia and Alzheimer’s: smoking, physical inactivity, high blood pressure, cholesterol and obesity.
Likewise, if the brain is damaged by a shock to the head, certain blood vessels will be broken and the risk of developing the disease will increase in the medium and long term. In other words, people who have had concussions are at a much higher risk of developing dementia or Alzheimer’s problems.
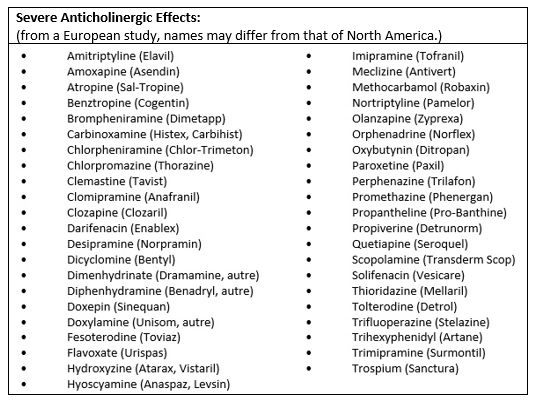
Anticholinergic drugs
Of course, not all drugs increase the risk of dementia and Alzheimer’s. Anticholinergics are the most important group of drugs for increasing the risk of dementia. These drugs act on the acetylcholine receptors; one of the most important neurotransmitters for the brain, but also for nerve transmission throughout the body. Many drugs have anticholinergic effects, classified from mild to severe. It is those who have a severe effect that increase the chances of developing the disease. These drugs would increase the risk of dementia by almost 50% if taken daily for three years or more. They are responsible for about 10% of the diagnosed cases.
We can add to this sleep problems, depression, poor glucose management, poor diet and taking certain medications (e.g. sleeping pills).
Despite all of this, remember that there are ways to prevent dementia and Alzheimer’s. In the next article on Alzheimer’s, we’ll take a closer look at what you can do now to lower your risk of getting the disease.
N.B.: It is very important to speak with your pharmacist or doctor before considering stopping a medication.
References:
- Blankevoort et al, 2013. Physical Predictors of Cognitive Performance in Healthy Older Adults: A Cross-Sectional Analysis. PLoS One. 2013 Jul 30; 8(7).
- Coupland et al, 2019. Anticholinergic Drug Exposure and the Risk of DementiaA Nested Case-Control Study. JAMA Intern Med. 2019;179(8):1084-1093.
- Harvard-health, Published by Harvard Medical School. 2018. Alzheimers disease a guide to diagnosis treatment and caregiving. David Roberts, MD, Dean for External Education, 53 pages.
- Harvard Men’s Health Watch, Décembre 2015, mise à jour Janvier 2019. Alzheimer’s in the family: Dementia affects the person diagnosed but also raises fears for siblings and children. Here are the facts. Harvard health publications.
- Henry et al, 2019. The relationship between sleep duration, cognition and dementia: a Mendelian randomization study. Int J Epidemiol. 2019 Jun 1;48(3):849-860.
- Pottie et al, 2018. Déprescription des agonistes des récepteurs des benzodiazépines. Guide de pratique clinique. Vol 64 : MAY | MAI 2018|Canadian Family Physician | Le Médecin de famille canadien. 16 pages.
- Samieri et al, 2018. Association of Cardiovascular Health Level in Older Age With Cognitive Decline and Incident Dementia, JAMA. 2018; 320(7):657-664.
- Wahlin and Nyberg, 2019. At the Heart of Cognitive Functioning in Aging. Trends in Cognitive Sciences July 11, 2019.






